Jaime was delivered after a traumatic 15-hour labor that almost ended up with an emergency cesarean. Despite expecting Jaime to make her appearance before her expected date of delivery, she ended up baking past her due date. I have been having the so-called braxton hicks contractions often since Week 37/38. There were times when I thought "that was it" but the contractions always subsided after a good warm bath, and I always manage to fall back asleep.
Week 38
I'm thankful to have 2 weeks of rest before delivery though as i started maternity leave from Week 38. Work was getting really busy and I was getting extremely tired towards the end. I spent my rest days sleeping in, napping and reading alot, trying to prepare myself mentally. I met with my September Mummy friends for high-tea and buffet on weekdays, in anticipation for our big days. Weekends were spent with the husband, enjoying the last days of just the two of us, preparing for Jaime's arrival.
Here's Jaime's room, the massage area in my study and the cosy corner in our room where I will spend many sleepless nights:

How did I grow so much?

Calm before the storm. Peaceful nights like that would be hard to come by soon.

Week 39
At my 39w2d gynae appointment, I made the decision to do an induction on 40w1d if Jaime was still not out by then. Despite being aware that induction increases the chance of an emergency cesarean and usually results in a longer labor, I thought that Jaime might as well share the same birthday as her father instead of waiting indefinitely. Our gynae is very pro-natural and finally did a cervix check since I've decided on induction. Thankfully, it was painless though uncomfortable. I was already 2-3cm dilated and the cervix was quite thin then. He was happy to schedule the induction for next week, but warned that baby may come sooner than that.
Nothing happened that week though, and the husband was on leave a day before my induction. Actually everything was somewhat a blur. We did the last minute preparations and I think I had everything I wanted to eat, did most of what I wanted to do. I had a long bath and prepared to check-in at midnight.
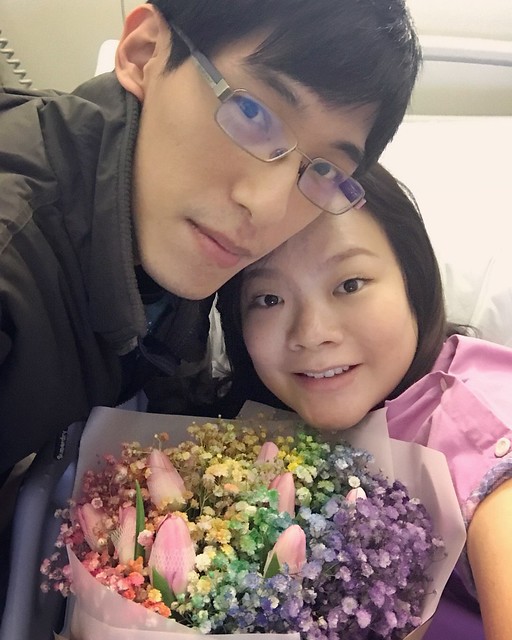
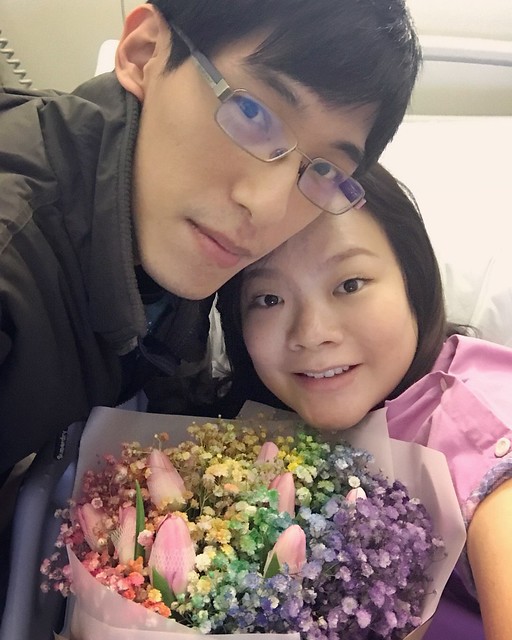
Celebrating the husband's birthday 3rd September in advance, because there's no knowing when I'll deliver:



Sending my sister off to her one-year exchange in Tokyo. She won't be able to see Jaime as a baby!

Those quiet afternoons with Chikey:

40 weeks and nearing the end of my pregnancy journey:

Jaime's nursery finally done up the day I'm due to be induced:

A photo right before we left for the hospital:

The Delivery
We arrived at Mount Alvernia's delivery ward at 1230am and was ushered to Delivery Room 6 to change into the hospital robe before being hooked on CTG. The husband went downstairs to register me (although we've pre-registered) and took a good long hour before coming. They finally checked my dilation again and inserted the pill for induction at 230am. I asked for the birthing ball since hospital confirmed that it's available for us by email. However, they told me that the ball was not usable because the air wasn't enough! I had to send the husband back to grab my ball! By 4am, I finally felt the first contractions in my lower abdomen. At 530am, the contractions became more frequent every 3-5 minutes, but was bearable as I bounced on the ball. The contractions were pretty unbearable while lying on the bed, but so much better on the ball.
My gyane finally came at 10am and broke my waterbag when I was about 4cm dilated. Warm water flowed out uncontrollably. It was then that things got real. He said that there was meconium in my amniotic fluid, but we can still try for vaginal delivery as babies don't usually inhale while in the tummy, unless distressed. He did mention that most doctors will usually do an emergency cesarean when they notice meconium, but medically, the chances of inhalation is very low. I have done enough reading to know what was at stake and the consequences, but was comfortable with the doctor's advice since I wanted to avoid a cesarean as much as possible. The contractions came in strong and frequent right after my waterbag burst. I can barely concentrate as the doctor continued talking. He briefed us about pain management and using laughing gas, and also said that he expected me to deliver in the evening, a good 8-10 hours more.
Barely half an hour after my waterbag burst, the contractions were really getting unbearable. The thought of having to go through this for a full day and a possibility of a cesarean made me decide to go for epidural. I didn't want to be on GA if I had to have a cesarean and being in so much pain for hours on end was unimaginable. I saw the look of concern when I asked the husband to get me an epidural, because he knew that I was hoping to go without. I was adamant though, and he went to request for it.
My anesthetist took awhile to come and he had shaking hands that I noticed even when I was in great pain. Thankfully, the administration was painless and over in barely 10 minutes or so and I didn't feel my contractions anymore. I was still able to move my legs and fell asleep right after. When I was awake, I started crying, because I was worried about the meconium and was afraid that something may happen to Jaime. The husband must have felt very helpless seeing me in that state and that was the start of my emotional roller coaster that lasted for days.
At 3pm, the nurse came to check and I was 7cm dilated, but baby was still quite high. By 4pm, my gynae was here and I was already more than 9cm dilated and expected to start pushing in an hour as baby descends. I started pushing at 5.40pm, and it was hard work. No matter how hard I tried to push, Jaime didn't seem to be moving down despite ample clearance. I was so thankful that I had epidural, because everytime I pushed, the nurse helped to stretch my cervix with her fingers quite forcefully. Luckily I didn't feel anything, but I could anticipate the soreness after.
After an hour of pushing, Jaime's heartbeat was getting irregular and our gynae was saying that I may need a cesarean if she still doesn't come out soon. I seriously pushed with all my might with every contraction while the doctor prepared forceps and gave me some pitocin to increase contraction strength. Jaime was finally out at 7pm sharp and she spluttered instead of wailing. They placed her on my lower tummy when she was out, and I remembered being scared because I felt her weight on me but she wasn't wailing like how babies are supposed to.
The pediatrician was already in the room when Jaime was out and quickly placed her on the heating area and gave her a thorough check. I was in despair as she was taken away and the husband didn't even get to cut the umbilical cord as meconium particles were noticed upon delivery. I looked on as my gynae helped to deliver my placenta by gently applying pressure to my lower abdomen. He started sewing me up and took almost 45 minutes as I suffered 4th degree tears. I couldn't feel the pain but can feel the stitches, and thought that I'm going to have a tough time recovering. Jaime was found to have a cleft palate, and she was heaving heavily. She had to be sent to NICU right after a quick photo with me (with the oxygen tube right near her nose). Lying there helpless was really one of the worst thing that could happen as everything I envisioned did not materialize.
The husband had to leave the delivery ward to do the admission for Jaime. By the time he's back, I was crying uncontrollably again. All the fear and pain was overwhelming, and I was worried sick. It was really upsetting that I didn't get any skin-to-skin nor managed to breastfeed Jaime upon delivery like I envisioned. The husband also didn't get to cut her cord nor did we get any time together in the delivery ward for bonding. I was feeling absolutely torn and spent by then, but still insisted that they keep dinner for me (hah!). The nurses was hesitant to serve me dinner although my gynae gave the green light. I insisted multiple times before they agreed to keep my dinner for me to eat later on. They were worried that I may regurgitate after food, but I was so hungry after going without food for 24 hours. I didn't even vomit since epidural was administered, only the laughing gas made me puke.
Jaime's first photo:

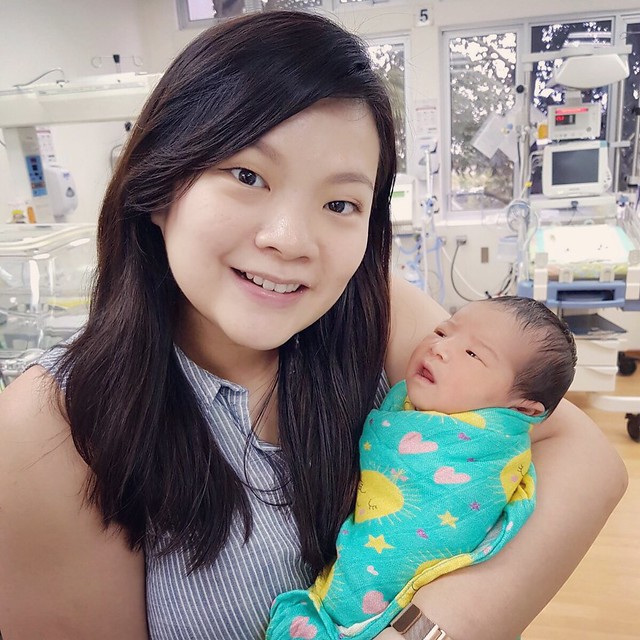
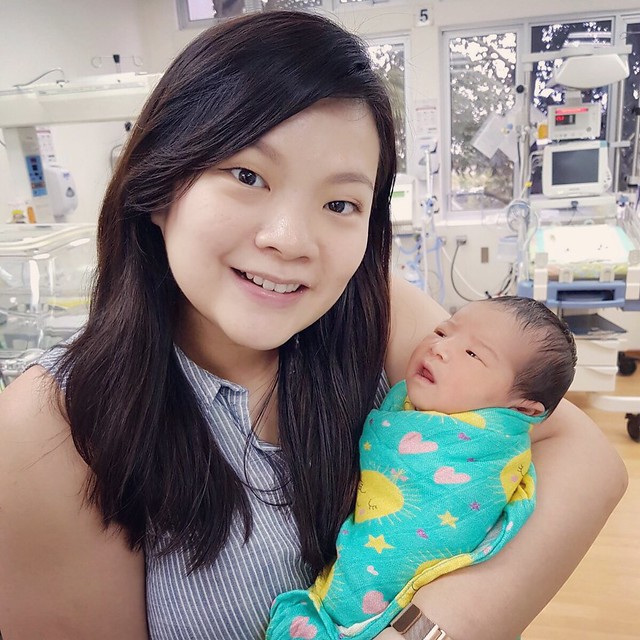
The first time I held Jaime:

Our first family photo:

Our parents came the first night, although I was totally not in the mood for visitors to see me in that state. It was almost 9pm by the time I got into my ward and I finally had dinner. I was totally spent and fell asleep right after the husband left. It was the first of few night that I feel asleep in tears, those were the dark days.
Jaime's first night all alone in NICU. To think I wanted to room-in with her after delivery.

By 3am the first night, I was famished again. I pressed the call bell for some milo, and the nurse came in asking if I'm done feeding baby - that triggered my tears again, because there was no baby. I couldn't feed my baby, I haven't even taken a good look at her nor cuddled her. The thought itself was overwhelmingly upsetting. The epidural has worn off by now and I was in pain. I was so thankful that the catheter was still in me as I can't imagine getting off bed nor touching down there. Even shifting my weight on the bed was painful and the nurses came to help change my pad and clean me up - very humiliating but necessary. I simply lay there in pain and the painkillers made me very drowsy and weak.
The gynae and PD came in the morning. Luckily the gynae took off my IV drip and kept my catheter for another day as my tear and inflammation was quite bad. Jaime was breathing better but they put her on antibiotics drip just in case as there seemed to be some particles in her lungs. The husband came shortly and knew how much I wanted to see Jaime. He actually got a wheelchair to push me to the NICU as they helped me get out of bed with my pee bag gingerly. It was excruciating seeing her hooked up in tubes. The nurses didn't let me carry her fearing that her IV needle may need to be reinserted. No mother would want to see her newborn in that state and not being able to carry nor feed her nor be with her right after delivery.
Jaime was breathing normally and off the oxygen hood the following day:

And my happy baby can still smile:

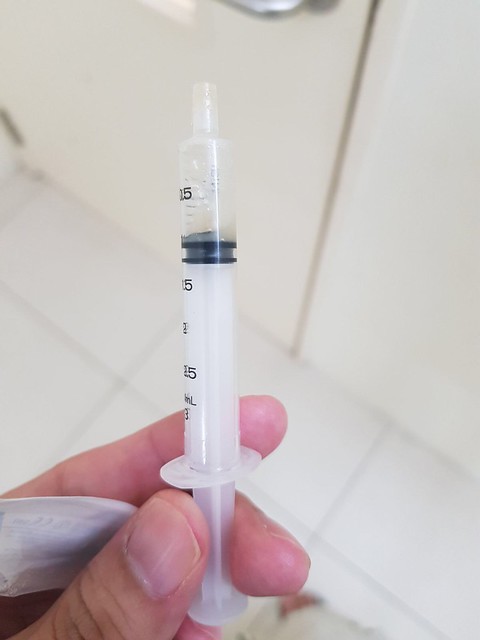
The lactation consultant came that day, and taught me how to squeeze colostrum for syringe collection. It hurt, but it gave me something to do for Jaime and I squeezed relentlessly that few days (and nights) and sent the little syringes up to the NICU.
The first few days were terrible. I was so emotional and felt terrible whenever I hear babies crying. Many things became triggers for my tears to flow. I cried myself to sleep everynight and some nurses told me they understood, to try not to cry. Some nurses saw my swollen eyes and was concerned if it was caused by drug allergies. There was once when my mum came and said things like latching my baby would help my uterus to shrink quickly - as if I didn't want to if I could! And pumping/hand-expressing was supposed to help shrink the uterus too. Then I totally lost it when she asked if I had enough breastmilk to store - it was the second day after delivery and I was struggling to squeeze barely few ml of colostrum, and here she was asking if I had enough to store. I started brawling again after she left, and the poor husband was at a loss again. He kept telling me Jaime was fine, but it was everything that I couldn't do and all the worries that was overwhelming for me. He was totally perfect and I knew there were many times when he held it in to be strong for me, for us.
My pillar of strength:
Thankfully, the dark days got better day-by-day. I slowly stopped crying as I focus on providing more breastmilk to feed Jaime. Then I got out of bed on the 3rd day and went to see her daily. They finally allowed me to carry her and feed her, and she would be discharged after 5 days of antibiotics drip.
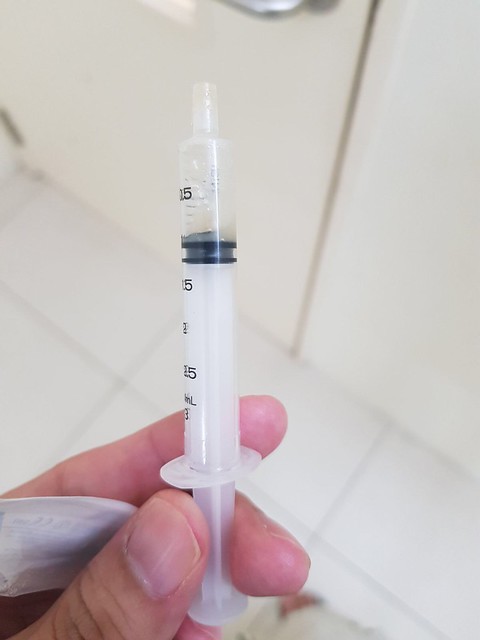
My first syringe of colostrum on the second day. The husband sent the syringe up to the NICU and took a photo of it saying 'good job'. On hindsight, this was quite pathetic but that 2 words meant so much then.
The second time I held her, the night before I was discharged. We sent up a syringe of colostrum and the nurse finally let me carry her.

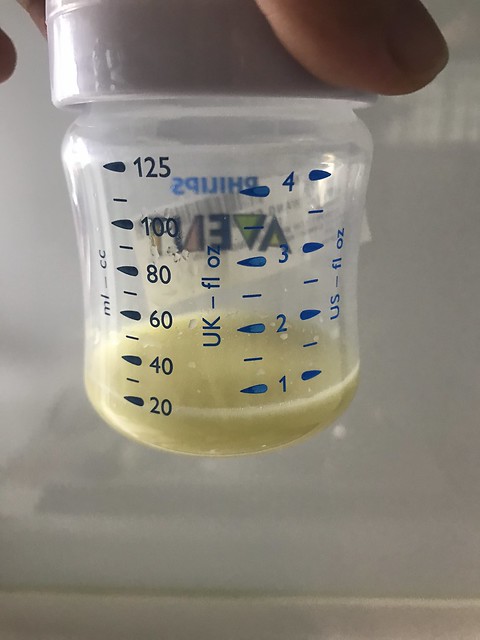
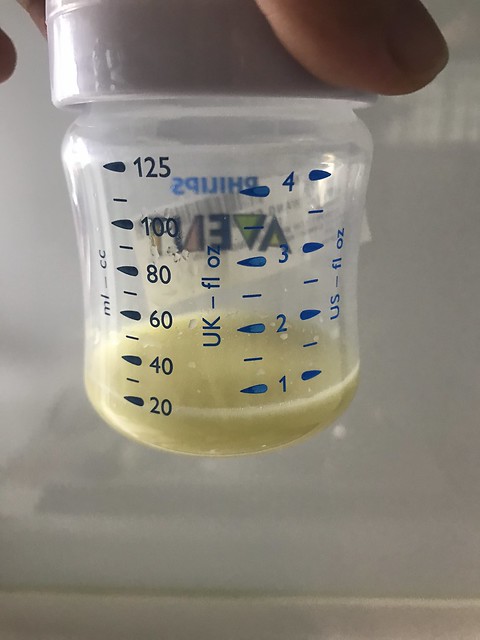
My first pump after being discharged at home:
Feeding her at the NICU:

My angel:

Finally bringing Jaime home:
A family photo for the record:

Jaime's first photo at home =)

Things could have been worst as there's really no knowing what could go wrong. I'm thankful that Jaime's safe and healthy, although having to send her for surgery at such a young age pains me greatly. I'm still not sure how I can go through that. We've come such a long way, from trying to conceive to finally getting pregnant and delivering her safely. There's still a long way to go and there's no doubt that we will try our best to be parents to Jaime.
The most difficult thing is not handling a newborn, it's having to handle all the comments and advice that everyone feels inclined to give. Everyone wants to have a say about what and how you do things, right down to what you ate and what you should not do. Eeryone thinks they know better and that you should follow what they say. Of course, everyone has good intentions, but it's really tiring. The hardest thing about motherhood is having to accept help because you can't do everything by yourself, and there are things that you have to compromise on.
From all of these, what my gynae said truly hit home. We were obviously concerned about what causes cleft palate and if there's any way to avoid or detect it the next pregnancy. He said that there's nothing we can do to avoid it, and detecting it may be difficult since it's deep within the mouth and not picked up by even tests like Harmony/Panorama. Also, since cleft palate babies are perfectly healthy and could even live normally without surgery, what could we do if we knew earlier? Nobody in the right mind would terminate the pregnancy just because of a cleft palate. He also said that we wouldn't know for sure how things will turn out for our children till the very end. Some babies are born with certain congenital diseases but go on to live perfectly normal lives, yet some are born perfectly healthy with issues coming up later on in life. Unless we choose not to have children, otherwise, these are things that we have to face and live with.
Here's to parenthood and a lifetime of worries~
Week 38
I'm thankful to have 2 weeks of rest before delivery though as i started maternity leave from Week 38. Work was getting really busy and I was getting extremely tired towards the end. I spent my rest days sleeping in, napping and reading alot, trying to prepare myself mentally. I met with my September Mummy friends for high-tea and buffet on weekdays, in anticipation for our big days. Weekends were spent with the husband, enjoying the last days of just the two of us, preparing for Jaime's arrival.
Here's Jaime's room, the massage area in my study and the cosy corner in our room where I will spend many sleepless nights:

How did I grow so much?

Calm before the storm. Peaceful nights like that would be hard to come by soon.

Week 39
At my 39w2d gynae appointment, I made the decision to do an induction on 40w1d if Jaime was still not out by then. Despite being aware that induction increases the chance of an emergency cesarean and usually results in a longer labor, I thought that Jaime might as well share the same birthday as her father instead of waiting indefinitely. Our gynae is very pro-natural and finally did a cervix check since I've decided on induction. Thankfully, it was painless though uncomfortable. I was already 2-3cm dilated and the cervix was quite thin then. He was happy to schedule the induction for next week, but warned that baby may come sooner than that.
Nothing happened that week though, and the husband was on leave a day before my induction. Actually everything was somewhat a blur. We did the last minute preparations and I think I had everything I wanted to eat, did most of what I wanted to do. I had a long bath and prepared to check-in at midnight.
Celebrating the husband's birthday 3rd September in advance, because there's no knowing when I'll deliver:



Sending my sister off to her one-year exchange in Tokyo. She won't be able to see Jaime as a baby!

Those quiet afternoons with Chikey:

40 weeks and nearing the end of my pregnancy journey:

Jaime's nursery finally done up the day I'm due to be induced:

A photo right before we left for the hospital:

The Delivery
We arrived at Mount Alvernia's delivery ward at 1230am and was ushered to Delivery Room 6 to change into the hospital robe before being hooked on CTG. The husband went downstairs to register me (although we've pre-registered) and took a good long hour before coming. They finally checked my dilation again and inserted the pill for induction at 230am. I asked for the birthing ball since hospital confirmed that it's available for us by email. However, they told me that the ball was not usable because the air wasn't enough! I had to send the husband back to grab my ball! By 4am, I finally felt the first contractions in my lower abdomen. At 530am, the contractions became more frequent every 3-5 minutes, but was bearable as I bounced on the ball. The contractions were pretty unbearable while lying on the bed, but so much better on the ball.
My gyane finally came at 10am and broke my waterbag when I was about 4cm dilated. Warm water flowed out uncontrollably. It was then that things got real. He said that there was meconium in my amniotic fluid, but we can still try for vaginal delivery as babies don't usually inhale while in the tummy, unless distressed. He did mention that most doctors will usually do an emergency cesarean when they notice meconium, but medically, the chances of inhalation is very low. I have done enough reading to know what was at stake and the consequences, but was comfortable with the doctor's advice since I wanted to avoid a cesarean as much as possible. The contractions came in strong and frequent right after my waterbag burst. I can barely concentrate as the doctor continued talking. He briefed us about pain management and using laughing gas, and also said that he expected me to deliver in the evening, a good 8-10 hours more.
Barely half an hour after my waterbag burst, the contractions were really getting unbearable. The thought of having to go through this for a full day and a possibility of a cesarean made me decide to go for epidural. I didn't want to be on GA if I had to have a cesarean and being in so much pain for hours on end was unimaginable. I saw the look of concern when I asked the husband to get me an epidural, because he knew that I was hoping to go without. I was adamant though, and he went to request for it.
My anesthetist took awhile to come and he had shaking hands that I noticed even when I was in great pain. Thankfully, the administration was painless and over in barely 10 minutes or so and I didn't feel my contractions anymore. I was still able to move my legs and fell asleep right after. When I was awake, I started crying, because I was worried about the meconium and was afraid that something may happen to Jaime. The husband must have felt very helpless seeing me in that state and that was the start of my emotional roller coaster that lasted for days.
At 3pm, the nurse came to check and I was 7cm dilated, but baby was still quite high. By 4pm, my gynae was here and I was already more than 9cm dilated and expected to start pushing in an hour as baby descends. I started pushing at 5.40pm, and it was hard work. No matter how hard I tried to push, Jaime didn't seem to be moving down despite ample clearance. I was so thankful that I had epidural, because everytime I pushed, the nurse helped to stretch my cervix with her fingers quite forcefully. Luckily I didn't feel anything, but I could anticipate the soreness after.
After an hour of pushing, Jaime's heartbeat was getting irregular and our gynae was saying that I may need a cesarean if she still doesn't come out soon. I seriously pushed with all my might with every contraction while the doctor prepared forceps and gave me some pitocin to increase contraction strength. Jaime was finally out at 7pm sharp and she spluttered instead of wailing. They placed her on my lower tummy when she was out, and I remembered being scared because I felt her weight on me but she wasn't wailing like how babies are supposed to.
The pediatrician was already in the room when Jaime was out and quickly placed her on the heating area and gave her a thorough check. I was in despair as she was taken away and the husband didn't even get to cut the umbilical cord as meconium particles were noticed upon delivery. I looked on as my gynae helped to deliver my placenta by gently applying pressure to my lower abdomen. He started sewing me up and took almost 45 minutes as I suffered 4th degree tears. I couldn't feel the pain but can feel the stitches, and thought that I'm going to have a tough time recovering. Jaime was found to have a cleft palate, and she was heaving heavily. She had to be sent to NICU right after a quick photo with me (with the oxygen tube right near her nose). Lying there helpless was really one of the worst thing that could happen as everything I envisioned did not materialize.
The husband had to leave the delivery ward to do the admission for Jaime. By the time he's back, I was crying uncontrollably again. All the fear and pain was overwhelming, and I was worried sick. It was really upsetting that I didn't get any skin-to-skin nor managed to breastfeed Jaime upon delivery like I envisioned. The husband also didn't get to cut her cord nor did we get any time together in the delivery ward for bonding. I was feeling absolutely torn and spent by then, but still insisted that they keep dinner for me (hah!). The nurses was hesitant to serve me dinner although my gynae gave the green light. I insisted multiple times before they agreed to keep my dinner for me to eat later on. They were worried that I may regurgitate after food, but I was so hungry after going without food for 24 hours. I didn't even vomit since epidural was administered, only the laughing gas made me puke.
Jaime's first photo:

The first time I held Jaime:

Our first family photo:

Our parents came the first night, although I was totally not in the mood for visitors to see me in that state. It was almost 9pm by the time I got into my ward and I finally had dinner. I was totally spent and fell asleep right after the husband left. It was the first of few night that I feel asleep in tears, those were the dark days.
Jaime's first night all alone in NICU. To think I wanted to room-in with her after delivery.

By 3am the first night, I was famished again. I pressed the call bell for some milo, and the nurse came in asking if I'm done feeding baby - that triggered my tears again, because there was no baby. I couldn't feed my baby, I haven't even taken a good look at her nor cuddled her. The thought itself was overwhelmingly upsetting. The epidural has worn off by now and I was in pain. I was so thankful that the catheter was still in me as I can't imagine getting off bed nor touching down there. Even shifting my weight on the bed was painful and the nurses came to help change my pad and clean me up - very humiliating but necessary. I simply lay there in pain and the painkillers made me very drowsy and weak.
The gynae and PD came in the morning. Luckily the gynae took off my IV drip and kept my catheter for another day as my tear and inflammation was quite bad. Jaime was breathing better but they put her on antibiotics drip just in case as there seemed to be some particles in her lungs. The husband came shortly and knew how much I wanted to see Jaime. He actually got a wheelchair to push me to the NICU as they helped me get out of bed with my pee bag gingerly. It was excruciating seeing her hooked up in tubes. The nurses didn't let me carry her fearing that her IV needle may need to be reinserted. No mother would want to see her newborn in that state and not being able to carry nor feed her nor be with her right after delivery.
Jaime was breathing normally and off the oxygen hood the following day:

And my happy baby can still smile:

The lactation consultant came that day, and taught me how to squeeze colostrum for syringe collection. It hurt, but it gave me something to do for Jaime and I squeezed relentlessly that few days (and nights) and sent the little syringes up to the NICU.
The first few days were terrible. I was so emotional and felt terrible whenever I hear babies crying. Many things became triggers for my tears to flow. I cried myself to sleep everynight and some nurses told me they understood, to try not to cry. Some nurses saw my swollen eyes and was concerned if it was caused by drug allergies. There was once when my mum came and said things like latching my baby would help my uterus to shrink quickly - as if I didn't want to if I could! And pumping/hand-expressing was supposed to help shrink the uterus too. Then I totally lost it when she asked if I had enough breastmilk to store - it was the second day after delivery and I was struggling to squeeze barely few ml of colostrum, and here she was asking if I had enough to store. I started brawling again after she left, and the poor husband was at a loss again. He kept telling me Jaime was fine, but it was everything that I couldn't do and all the worries that was overwhelming for me. He was totally perfect and I knew there were many times when he held it in to be strong for me, for us.
My pillar of strength:
Thankfully, the dark days got better day-by-day. I slowly stopped crying as I focus on providing more breastmilk to feed Jaime. Then I got out of bed on the 3rd day and went to see her daily. They finally allowed me to carry her and feed her, and she would be discharged after 5 days of antibiotics drip.
My first syringe of colostrum on the second day. The husband sent the syringe up to the NICU and took a photo of it saying 'good job'. On hindsight, this was quite pathetic but that 2 words meant so much then.
The second time I held her, the night before I was discharged. We sent up a syringe of colostrum and the nurse finally let me carry her.

My first pump after being discharged at home:
Feeding her at the NICU:

My angel:

Finally bringing Jaime home:
A family photo for the record:

Jaime's first photo at home =)

Things could have been worst as there's really no knowing what could go wrong. I'm thankful that Jaime's safe and healthy, although having to send her for surgery at such a young age pains me greatly. I'm still not sure how I can go through that. We've come such a long way, from trying to conceive to finally getting pregnant and delivering her safely. There's still a long way to go and there's no doubt that we will try our best to be parents to Jaime.
The most difficult thing is not handling a newborn, it's having to handle all the comments and advice that everyone feels inclined to give. Everyone wants to have a say about what and how you do things, right down to what you ate and what you should not do. Eeryone thinks they know better and that you should follow what they say. Of course, everyone has good intentions, but it's really tiring. The hardest thing about motherhood is having to accept help because you can't do everything by yourself, and there are things that you have to compromise on.
From all of these, what my gynae said truly hit home. We were obviously concerned about what causes cleft palate and if there's any way to avoid or detect it the next pregnancy. He said that there's nothing we can do to avoid it, and detecting it may be difficult since it's deep within the mouth and not picked up by even tests like Harmony/Panorama. Also, since cleft palate babies are perfectly healthy and could even live normally without surgery, what could we do if we knew earlier? Nobody in the right mind would terminate the pregnancy just because of a cleft palate. He also said that we wouldn't know for sure how things will turn out for our children till the very end. Some babies are born with certain congenital diseases but go on to live perfectly normal lives, yet some are born perfectly healthy with issues coming up later on in life. Unless we choose not to have children, otherwise, these are things that we have to face and live with.
Here's to parenthood and a lifetime of worries~
No comments:
Post a Comment